Revenue cycle management for ALL Specialties
Revenue cycle management for ALL Specialties
Medical Billing Consultants Specialize in Healthcare Revenue Cycle Management.
Medical Billing Consultants Specialize in Healthcare Revenue Cycle Management.
Medical Billing Consultants employs some of the most experienced billers in the medical profession and we have perfected the science of medical billing coding. Personal accountability and intimate customer care are part of our core values. Outsourcing your medical billing is smart. Let our team of experts get you paid more, and get paid fast.
YOUR SYSTEM OR OURS
YOUR SYSTEM OR OURS
No need to change systems for MBC to provide our services.
EXPERTISE
EXPERTISE
Our only focus is maximizing your practice’s profit. Our team stays apprised of insurance rules and regulations. Medical Billing Consultants collects 97.4% of medical billing collectable revenue in an average of 21.4 days for the clients we serve. MBC will audit and submit clean, accurate claims within 48 hours. Every claim is professionally verified and personally tracked.
OUR STAFF IS YOUR STAFF
OUR STAFF IS YOUR STAFF
We are a dependable, powerful resource that works as a team with your internal staff to provide support and training in your medical practice.
Benefits of Outsourcing Billing
DEDICATED EXPERTS.
Our team only has one purpose, to increase the profitability of your practice. Your practice gains access to a large combined knowledge base of billing experts. Keeping up with the ever changing rules and requirements is difficult.
GET PAID FASTER
Our team will submit your claims faster and with fewer error. Claims are scrubbed multiple times to ensure correct submission the first time. Our experts utilize efficient policies and procedures to reduce your cycle time.
Our team only has one purpose, to increase the profitability of your practice. Your practice gains access to a large combined knowledge base of billing experts. Keeping up with the ever changing rules and requirements is difficult.
GET PAID FASTER
Our team will submit your claims faster and with fewer error. Claims are scrubbed multiple times to ensure correct submission the first time. Our experts utilize efficient policies and procedures to reduce your cycle time.
CONSISTENCY.
In house billing puts your cash flow at risk for revenue interruptions due to employee absence or staff turnover.
FOCUS ON WHAT YOU DO BEST – Patient Care.
In house billing requires a lot of time and effort. Our expert billers are privy to aggregated trends from a network of other practices. This inside information keeps them on the forefront.
The features below are included in our revenue cycle management service.
Credentialing
We will assume your credentialing responsibilities from day one. We have years of expertise in working with countless payers and specialties from across the country.
We also utilize software and technology to eliminate the potential for stalled claims.
Coding and Compliance
Our Coding and Compliance team is comprised of in-house, certified coding expertise in conjunction with cutting-edge, computer-assisted word recognition technology. We will implement a compliance program that consists of continual in-house quality assurance audits, but also includes an annual “third party” auditing process to ensure maximum compliance levels.
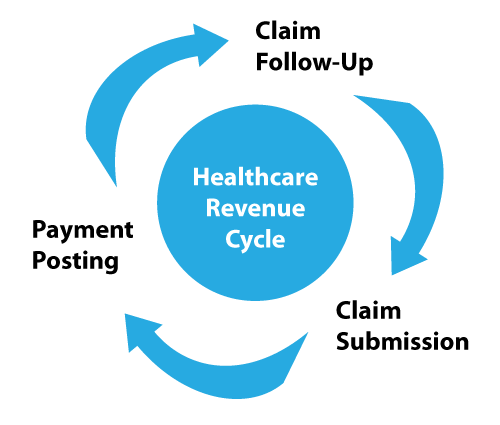
Claim Submission
We provide direct electronic processing (EDI) of claims to all major payers. We also have access to submit to those payers that do not support direct submission.
There are no clearinghouse costs passed to your practice, and we submit claims in a timely manner in accordance with established standards.
Payment Posting
Our posts and deposits payments timely and accurately for immediate balancing and deposit verification. EOBs are scanned and indexed for easy retrieval and efficient denial management. We have processes in place to review payers for ERA (Electronic Remittance Advice) and EFT (Electronic Funds Transfer) capabilities, so you receive your payments faster.
Contract Variance
We provide an insurance contract variance solution to verify that your current reimbursement levels are accurate. Our enterprise-level revenue cycle management software is capable of measuring these variances instantly. Contract variance can increase revenue, but also proactively identify and avoid mass recoupment liability.
The Start Up / Go Live
Our client Start Up process is well documented and defined. We take a very “hands on” approach to implement the plan and create process continuity between us.
Our shared goal is to smoothly transition you to our solutions, while simultaneously keeping your cash flow stabilized.
Charge Capture
We have built processes to capture all charges efficiently whether we receive them electronically or on paper. Pollux will take the extra steps to capture and charge all services provided by the practice. We understand the importance of obtaining the correct information on the front end to eliminate stalls on the back end.
A/R Management
Our Insurance Resolution process is aggressive, highly detailed and effective in tracking denials, overseeing files and receiving a timely response. We have developed specific software tools and processes to effectively manage and reduce denials, thus improving your practice’s payment cycle and cash flow. We electronically batch all denials and non-response claims into Stalled Claims Service Centers. These Service Centers are worked daily in accordance with well-defined throughput standards.